This set of Molecular Endocrinology Multiple Choice Questions & Answers (MCQs) focuses on “Mechanism of Action of Glucocorticoids”.
1. Where is the glucocorticoid receptor protein found in the cell?
a) Cytosol
b) Nucleus
c) Endoplasmic Reticulum
d) Ribosomes
View Answer
Explanation: Through the plasma membrane, glucocorticoids migrate into target cells and bind to particular glucocorticoid receptor proteins found in the cytosol. In a wide range of target tissues such as liver, muscles, adipose tissue, lymphoid tissue, skin, bone, fibroblasts, etc., these receptors are present.
2. What is the difference between alpha form and beta form of glucocorticoid receptors?
a) Different amino acid sequence in the N-terminal
b) Different amino acid sequence in the C-terminal
c) Different binding substrates
d) Difference in the number of domains
View Answer
Explanation: There are two types of glucocorticoid receptors in human beings which are alpha and beta forms. They differ in the amino acid sequence at their C-terminal end. Two forms of GR in humans, known as α and β, exist due to alternative mRNA splicing.
3. Which among the following, is a glucocorticoid receptor domain that is present in the N terminal end?
a) Steroid binding domain
b) DNA binding domain
c) Transcription-activating domain
d) L domain
View Answer
Explanation: Glucocorticoid receptor molecule has three domains in total. The transcription activating domain is present in the N terminal side of this molecule. The glucocorticoid receptor (GR) is a superfamily protein evolutionally retained by the nuclear receptor that mediates the various activities of glucocorticoids as a transcription factor dependent on ligands.
4. All of the steroid hormones act initially at the level of cell nucleus.
a) True
b) False
View Answer
Explanation: All steroids function predominantly at the cell nucleus (‘nuclear’ action) level. This action is to improve m-RNA synthesis and protein synthesis. Steroid hormones in the cytoplasm bind to receptors that form homodimers or heterodimers, migrate to the nucleus, and serve as nuclear receptors and factors of transcription.
5. In humans there are three types of glucocorticoid receptor proteins.
a) True
b) False
View Answer
Explanation: There are two kinds of receptor proteins in humans. The alpha form contains about 777 amino acids and the beta form contains 742 amino acids. The receptor to which cortisol and other glucocorticoids bind is a glucocorticoid receptor (GR, or GCR), also known as NR3C1 (Nuclear Receptor Subfamily3, Group C, Member 1).
6. Which is the heats shock protein that binds to the glucocorticoid receptor when the hormone is absent?
a) Hsp 27
b) Hap 90
c) Hsf 1
d) Hsp 90
View Answer
Explanation: In the absence of hormones, a heat-shock protein, hsp90, binds to the receptor. This helps to avoid folding of the receptor protein into its active conformation. Heat shock proteins (HSPs) are specific proteins that are made when cells are briefly exposed to temperatures above their normal growth temperature.
7. What causes the dissociation of Hsp 90 heat shock protein that binds to the glucocorticoid receptor?
a) Binding of glucocorticoid
b) Binding of the substrate
c) Binding of ACTH
d) Binding of mineralocorticoids
View Answer
Explanation: Glucocorticoids bind to the steroid-binding site of a specific receptor in the cytosol. This binding causes the ‘hsp90’ stabilizer to dissociate and allows the conversion into its active configuration.
8. In the nucleus, the DNA binding domain of the glucocorticoid receptor binds to which molecule?
a) Cortisol
b) C terminal proteins
c) Hsp 90
d) Hormone responsive element (HRE)
View Answer
Explanation: The steroid-receptor complex enters the nucleus and binds to the Hormone Responsive Element (HRE) of specific nuclear genes through the DNA binding site. The transcription rate of these genes is modulated by this process, leading to increased synthesis of many proteins.
9. What happens in a condition of steroid “resistance” occurring in fibroblasts and lymphoid cells?
a) Decreased sensitivity to steroids
b) Steroids are broken down
c) Steroids are inactivated
d) Steroids are activated
View Answer
Explanation: In different cells, the levels of specific receptors vary and can decrease in clinical conditions that cause decreased sensitivity to steroids. One among such conditions is the steroids “resistance” occurring in fibroblasts and lymphoid cells.
10. In the diagram given below, which shows the glucocorticoid mechanism, what is the molecule that is binding to the receptor domains?
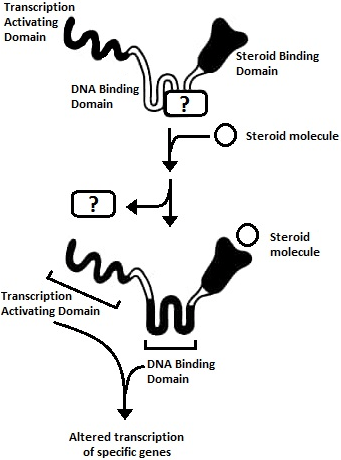
a) Cortisol
b) Hsp 90
c) ACTH
d) Hormone Responsive Element (HRE)
View Answer
Explanation: The polypeptide glucocorticoid receptor is represented schematically as a protein with three distinct domains. In the absence of a hormone, a heat-shock protein, hsp90, binds to the receptor and inhibits folding into the active protein.
11. What is the condition of steroids in diseased states like liver cirrhosis?
a) Mineralocorticoids are completely inactivated
b) Glucocorticoids are completely inactivated
c) Mineralocorticoids are not completely inactivated
d) Glucocorticoids are not completely inactivated
View Answer
Explanation: The liver does not completely inactivate “mineralocorticoids” in chronic liver disorders such as liver cirrhosis and congestive heart failure. This results in prolonged accumulation of sodium, which is responsible for the oedema and ascites present at some levels of these diseases.
12. Which adrenal androgen is derived from Dehydroepiandrosterone (DHEA)?
a) DHEA-SO4
b) 11-β-OH-androstenedione
c) Kinin
d) Δ4-androstenedione
View Answer
Explanation: Δ4-androstenedione is a DHEA derivative. Androstenedione is the precursor to a more potent male hormone, testosterone. Steroid hormones with poor androgenic activity are adrenal androgens (AAs), usually secreted by the foetal adrenal zone and the zona reticularis of the adrenal cortex.
13. In liver the androgens DHEA and all Δ4-androstenedione are converted to which among the following molecules?
a) Androsterone
b) DHEA-SO4
c) 11-β-OH-androstenedione
d) Kinin
View Answer
Explanation: Most of the DHEA and all Δ4-androstenedione are turned into androsterone and its isomer in the liver. It is also converted into Etiocholanolone. An endogenous steroid hormone, neurosteroid, and putative pheromone is Androsterone, or 3 alpha-hydroxy-5 alpha-androstan-17-one.
14. Which androgen is converted to 11-oxygenated derivatives of “androsterone” and ‘etiocholanolone?
a) Androsterone
b) DHEA-SO4
c) 11-β-OH-androstenedione
d) Kinin
View Answer
Explanation: 11-β-OH-androstenedione is the androgen that is converted into 11-oxygenated derivatives of androsterone and ‘etiocholanolone’. Both of them are sulphates or glucuronides conjugated molecules.
15. What is the blood level of corticosteroids in diseased states like renal failure?
a) Increased
b) Decreased
c) Remains the same
d) Absent
View Answer
Explanation: Corticoid inactivation declines during prolonged starvation and in disorders such as renal insufficiency. The blood volume of corticosteroids is elevated in these diseased conditions. The last stage of chronic kidney disease is renal failure, also called as end-stage renal disease (ESRD).
Sanfoundry Global Education & Learning Series – Molecular Endocrinology.
To practice all areas of Molecular Endocrinology, here is complete set of 1000+ Multiple Choice Questions and Answers.
If you find a mistake in question / option / answer, kindly take a screenshot and email to [email protected]
